Whether you’re just beginning your journey into the world of medical billing for mental health services, or you’re looking to make a switch, there are a number of important factors you’ll want to keep in mind. These factors include diagnosis coding, reimbursement rates, and double-checking patient insurance.
CPT codes
Using the right CPT codes for medical billing for mental health services is essential to getting paid. However, this can be a confusing process. Using the wrong codes can cause your claims to be denied and delay reimbursement. If you are uncertain of the codes you should be using, it is best to consult with an experienced medical billing company.
There are four categories of CPT codes for mental health services. Each of these categories is specific to a type of service. They are diagnostic interview, psychotherapy, assessment, and management. Depending on the type of service, you may be required to bill for different codes.
Psychotherapy codes include individual, family, and group services. Individual psychotherapy must include at least 45 minutes of face-to-face time. It must also be in an outpatient facility, and insight-oriented.
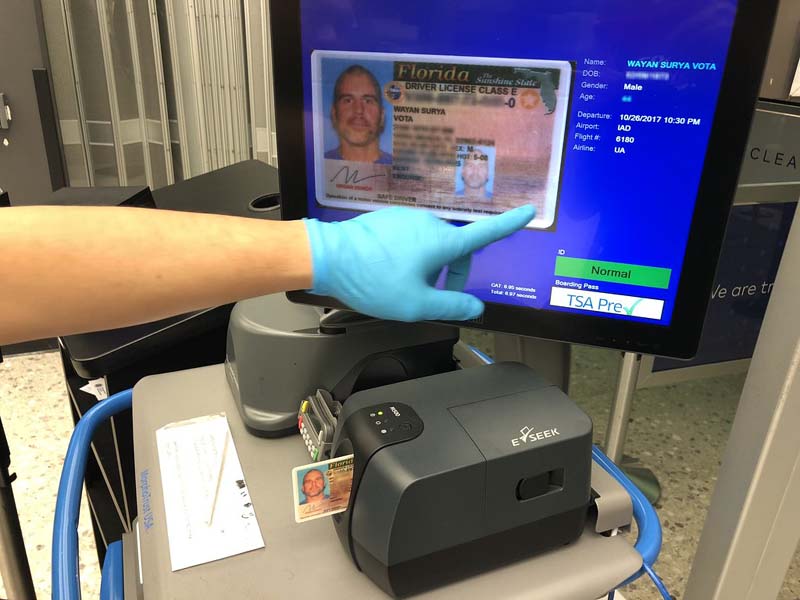
Double-checking patient insurance
Having an understanding of double-checking patient insurance when billing mental health services can be a lifesaver. In some cases, it can save time and effort by avoiding unnecessary claim rejections.
In other cases, it can be the difference between getting paid and not getting paid. The best way to do this is to check with the insurance company ahead of time. In some cases, the company will only reimburse services if a certain criteria is met. In other cases, a health plan will not pay for the actual treatment.
It is not uncommon for patients to forget to inform their doctors about changes in their insurance. It is also not uncommon for health insurance companies to require pre-authorization before a provider can see a patient. This can delay billing and prevent a patient from receiving the treatment they need.
Reimbursement rates
Whether you are a psychiatrist, psychologist, or counselor, understanding how insurance reimbursement rates work can help you get more money for your services. The insurance industry is constantly changing, so it’s important to be up-to-date on the latest rates and policies.
The most important thing to remember is that not all providers get paid the same rate. For example, a psychiatrist is usually reimbursed at a higher rate than a therapist.
One of the largest reasons why providers aren’t getting the reimbursement they deserve is cost. Some states have very specific guidelines for how to bill. It’s also important to understand that insurance reimbursement rates can change without notice.
There are two basic types of insurance reimbursement: Medicaid and Medicare. Medicaid provides health coverage to low-income individuals and is the largest payer for behavioral health services. Medicare, on the other hand, is a federal program administered by CMS.
Psychiatric therapeutic services
Psychiatric therapeutic services include both individual and group psychotherapy. Treatments may include behavioral modification, insight-oriented therapy, or crisis therapy.
There are many factors that determine how much insurance companies will reimburse for mental health services. This is due to the nature of the services. The length of time spent in a session can also affect coding.
Insurance companies have attempted to standardize mental health billing. However, errors can lead to problems with claims. It is vital to know the proper codes for psychiatric therapeutic services.
CPT codes are used to describe the exact service that is being provided. They are five digit numeric codes. Typically, they are used in conjunction with ICD codes. These codes are part of the International Classification of Diseases.
Many health plans require pre-authorization for mental health services. This pre-authorization can take a long time and may also delay the billing process.
Diagnosis coding
Using accurate diagnosis coding for mental health services can help to ensure that you are reimbursed for your work. In addition, using accurate codes can help to avoid claim denials. Having a good knowledge of the codes and guidelines is important to ensure that you are able to get the best reimbursement rates possible.
For example, in addition to using the appropriate ICD-10 diagnosis code, you should also include the appropriate E/M service code. There are several different E/M codes to choose from for mental health services. These include Z04.6, which is for a general psychiatric examination.
Other ICD-10 codes for mental health services include F32.9, which describes a major depressive disorder. F41.9 describes an unspecified anxiety disorder.
When you are preparing documentation for these services, you should include the following: an applicable diagnosis, a clinical impression, and the treatment objectives and outcomes. You should also include relevant history and test results. You should also include instructions for the patient to follow.